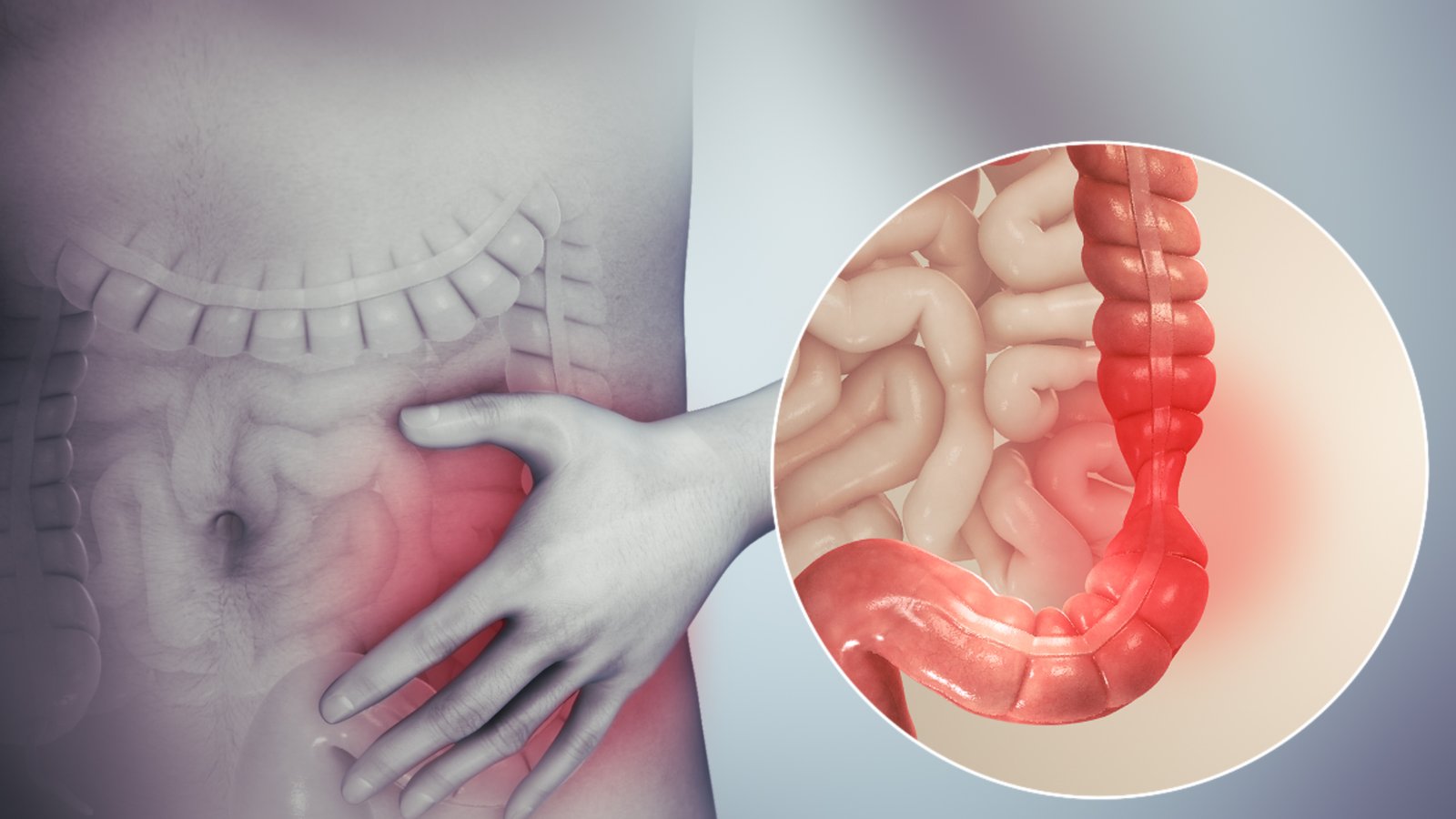
Irritable Bowel Syndrome (IBS) is a functional bowel disorder that causes recurrent abdominal discomfort, bloating, and altered bowel habits without structural damage to the intestine.
Though not life‑threatening, IBS can significantly affect daily life, productivity, and emotional wellbeing if not managed with a structured, personalised plan.
Common Symptoms
IBS symptoms can vary between individuals, but commonly include:

- Recurrent abdominal pain or cramping
- Bloating and gas
- Constipation, diarrhoea, or alternating pattern
- Relief of pain after passing stool
- Sense of incomplete evacuation
Causes & Diagnosis
IBS is linked to gut sensitivity, altered motility, stress, and gut‑brain axis imbalance rather than a single cause.
Cause
Primary Contributors
Stress, infections, food triggers, altered gut bacteria, and visceral hypersensitivity
Diagnosis
Diagnostic Methods
Clinical evaluation, basic blood and stool tests, and endoscopy when needed to rule out other diseases
Treatment
Treatment Approach
Dietary guidance, gut‑directed medicines, probiotic support, stress management, and long‑term lifestyle planning
Patient Outcomes
With a personalised, holistic approach, most IBS patients experience sustained symptom control and improved quality of life.
- Reduced episodes of pain and bloating
- More regular and comfortable bowel movements
- Better understanding of food and stress triggers
- Improved confidence in social and work settings
Ongoing follow‑up helps fine‑tune diet and treatment as symptoms fluctuate over time.
Frequently asked question
IBS tends to be long‑term, but symptoms can be very well controlled with diet, medicines, and stress management.
No, IBS does not cause cancer or structural damage, but it can significantly affect daily comfort if untreated.
Yes, certain foods can trigger or worsen symptoms, so a guided diet plan is an important part of IBS care.
Stress can strongly influence gut sensitivity; relaxation techniques, counselling, and adequate sleep often improve IBS symptoms.
